Table of Contents
ToggleProfessional Gynecological Services
Health:
It refers to the overall Professional Gynecological Services for the female reproductive system, including the uterus, ovaries, fallopian tubes, cervix, and vagina.
It encompasses various aspects such as menstrual health, reproductive health, and the prevention and detection of diseases and conditions affecting the female reproductive organs.
Significance for Women:
- Professional Gynecological Services is paramount to women of all ages as it directly impacts their reproductive capabilities, overall health, and quality of life.
- A healthy reproductive system is crucial for fertility, hormonal balance, and the prevention of gynecological diseases.
Importance of Regular Check-ups:
- Emphasize that regular Professional Gynecological Services are a cornerstone of women’s healthcare.
- Professional Gynecological Services including routine examinations, including pelvic exams and Pap smears, play a vital role in early detection of abnormalities or diseases, increasing the chances of successful treatment.
Preventive Care:
- Stress the significance of preventive care in maintaining gynecological health.
- Regular Professional Gynecological Services and vaccinations (such as the HPV vaccine) are key components of preventive care, helping to mitigate the risk of certain gynecological cancers and infections.

Common Gynecological Conditions:
-
Menstrual Disorders:
- Common menstrual disorders like irregular periods, heavy bleeding (menorrhagia), and painful periods (dysmenorrhea).
- Impact of these disorders on daily life and emphasize the importance of seeking medical advice for persistent issues.
-
Pelvic Pain:
- Different causes of pelvic pain, including menstrual cramps, pelvic inflammatory disease (PID), and endometriosis.
- Persistent or severe pelvic pain should be evaluated by a healthcare professional to determine the underlying cause.
-
Infections:
- Common gynecological infections include yeast infections, bacterial vaginosis, and sexually transmitted infections (STIs).
- Stress the importance of practicing safe sex, maintaining good hygiene, and seeking prompt medical attention for symptoms of infection.
-
Endometriosis:
- Endometriosis is a condition in which tissue similar to the lining of the uterus grows mainly outside the uterus.
- Advocate for early diagnosis and management through medical interventions and lifestyle modifications.
-
Polycystic Ovary Syndrome (PCOS):
- PCOS is a hormonal disorder affecting the ovaries, characterized by irregular periods, ovarian cysts, and hormonal imbalances.
- The potential long-term health implications and the importance of a multidisciplinary approach to manage symptoms.
-
Uterine Fibroids:
- Uterine fibroids as noncancerous growths in the uterus that can cause symptoms like heavy bleeding and pelvic pain.
Menstrual Health:
-
Menstrual Cycle and its Normal Variations:
- Menstrual Cycle Overview: The menstrual cycle is a regular, natural process that the female body undergoes in preparation for a potential pregnancy. On average, it lasts about 28 days, but variations are normal.
- Phases of the Menstrual Cycle: Break down the cycle into phases—menstrual, follicular, ovulatory, and luteal—and explain the hormonal changes and physical symptoms associated with each phase.
- Normal Variations: Emphasize that variations in cycle length, flow, and symptoms are common. Factors such as stress, diet, and exercise can influence the menstrual cycle.
-
Common Menstrual Disorders and Their Symptoms:
- Dysmenorrhea: Discuss menstrual cramps, their causes, and management strategies.
- Menorrhagia: Explore heavy menstrual bleeding, its potential causes, and available treatments.
- Amenorrhea: Address the absence of menstruation, its possible reasons (e.g., pregnancy, stress, hormonal imbalances), and when to seek medical advice.
- Premenstrual Syndrome (PMS): Highlight the emotional and physical symptoms that some women experience before menstruation.
-
Importance of Tracking Menstrual Health:
- Monitoring Menstrual Cycles: Encourage women to provide Professional Gynecological Services for their menstrual cycles using calendars or apps to identify patterns and irregularities.
- Early Detection of Issues: Explain how tracking can help detect irregularities early, enabling timely intervention for conditions like polycystic ovary syndrome (PCOS) or endometriosis.

Professional Gynecological Services for Reproductive Health and Family Planning:
-
Contraception Methods:
- Barrier Methods: Discuss options like condoms and diaphragms, highlighting their effectiveness in preventing pregnancy and STIs.
- Hormonal Methods: Explore birth control pills, patches, injections, and hormonal intrauterine devices (IUDs), explaining how they work and their potential side effects.
- Long-Acting Reversible Contraceptives (LARCs): Introduce options such as IUDs and implants, emphasizing their long-term effectiveness.
- Emergency Contraception: Provide information on the availability and proper use of emergency contraception.
-
Family Planning Options and Implications in Professional Gynecological Services:
- Natural Family Planning: Discuss Professional Gynecological Services like tracking ovulation and fertility awareness for couples wanting to conceive.
- Permanent Methods: Briefly mention sterilization options for individuals or couples who have completed their family planning.
- Implications and Considerations: Highlight the importance of open communication between partners, understanding the implications of chosen methods, and considering factors like age, health, and lifestyle.
Pregnancy and Prenatal Care:
Importance of Prenatal Care:
- Professional Gynecological Services involves medical supervision and support during pregnancy. Emphasize the importance of early and consistent prenatal care for both the mother’s and baby’s health.
- Regular check-ups help monitor the progress of the pregnancy, detect potential issues early, and ensure appropriate interventions are in place.
Common Issues During Pregnancy:
- Common issues related to pregnancy like morning sickness, gestational diabetes, and commonly high blood pressure.
- The changes in physical and emotional form that ladies may experience in the days of pregnancy.
Ways to Manage Pregnancy Issues:
- Get information on lifestyle changes and coping strategies to manage common pregnancy discomforts through Professional Gynecological Services
- Know the importance of a well-balanced diet, regular exercise, and adequate rest during pregnancy.
Sexual Health:
Encouraging Open Communication:
- Stress the importance of open communication between partners regarding sexual health.
- The significance of discussing sexual preferences, concerns, and any changes in sexual function.
- Encourage a supportive and non-judgmental environment for discussing intimate matters.
Safe Sex Practices:
- Various methods of contraception and family planning.
- The correct and consistent use of barrier methods, hormonal contraceptives, and other forms of birth control.
- The role of regular check-ups for sexual health, including screenings for STIs.
Prevention of STIs:
- The risks that are associated generally with sexually transmitted infections (STIs).
- The importance of practicing safe sex to prevent STIs and unintended pregnancies.
- Encourage routine STI screenings, especially for individuals with multiple partners or those entering new relationships.
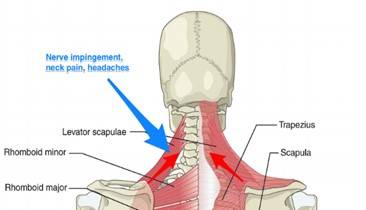
Pelvic Health:
- Significance of Pelvic Floor Health: The pelvic floor is a group of muscles, ligaments, and connective tissues that provide support to the pelvic organs, including the bladder, uterus, and rectum. Maintaining the health of the pelvic floor is crucial for various reasons. A strong and properly functioning pelvic floor helps in preventing urinary and fecal incontinence, supports reproductive organs, and contributes to sexual function. It also plays a vital role in maintaining posture and stability.
- Pelvic Floor Exercises and Their Benefits in Professional Gynecological Services: Pelvic floor exercises, commonly known as Kegel exercises, are designed to strengthen the muscles of the pelvic floor. These exercises involve contracting and relaxing the pelvic muscles to improve their tone and endurance.
- Preventing Incontinence: Strengthening the pelvic floor helps control bladder and bowel function, reducing the risk of incontinence.
- Enhancing Sexual Function: Improved pelvic muscle tone can enhance sexual satisfaction and may alleviate certain sexual dysfunctions.
- Supporting Reproductive Health: Pelvic floor exercises are beneficial during pregnancy and postpartum to support the growing uterus and aid in recovery after childbirth.
Postmenopausal Health focused on Professional Gynecological Services
- Health Considerations for Women Post-Menopause: Postmenopause is a stage in a woman’s life that begins after she has not menstruated for 12 consecutive months. During this phase, hormonal changes, particularly a decline in estrogen levels, can lead to various health considerations. These may include:
- Bone Health: The decrease in estrogen levels can contribute to bone density loss, increasing the risk of osteoporosis.
- Heart Health: Postmenopausal women may experience changes in cholesterol levels and an increased risk of cardiovascular diseases.
- Hormonal Changes and Their Effects on Health: Estrogen, the primary female sex hormone, significantly decreases during and after menopause. This hormonal shift can impact various aspects of health:
- Bone Density: Estrogen helps maintain bone density, and its decline can lead to an increased risk of fractures and osteoporosis.
- Cardiovascular Health: Estrogen has cardio-protective effects, and its reduction may contribute to an elevated risk of heart disease.
- Mood Changes: Hormonal fluctuations can influence mood and contribute to symptoms like irritability and mood swings.
Mental Health and Gynecology:
- Connection Between Gynecological Health and Mental Well-being: The relationship between gynecological health and mental well-being is intricate. Gynecological conditions, hormonal changes, and reproductive health experiences can impact mental health in various ways. Factors include:
- Chronic Conditions: Women dealing with chronic gynecological conditions may experience stress, anxiety, or depression.
- Reproductive Challenges: Infertility, pregnancy loss, or hormonal imbalances can have emotional implications.
- Hormonal Influence: Fluctuations in hormones, especially during menstruation, pregnancy, and menopause, can affect mood and mental health.
- Impact of Hormonal Changes on Mood and Mental Health: Hormonal changes, such as those occurring during the menstrual cycle, pregnancy, and menopause, can influence mood and mental well-being:
- Premenstrual Syndrome (PMS): Hormonal fluctuations before menstruation can lead to symptoms like mood swings, irritability, and anxiety.
- Menopausal Transition: Hormonal fluctuations during menopause may be associated with mood changes and an increased risk of mood disorders.
Importance of Regular Check-ups:
Emphasize the need for routine Professional Gynecological Services:
- Regular gynecological exams are crucial for maintaining women’s health and preventing potential issues. They allow healthcare providers to detect and address concerns early on.
- These exams typically include a pelvic exam, Pap smear, breast examination, and discussions about reproductive health. Emphasize that these routine Professional Gynecological Services play a key role in early detection and prevention.
Guide when to seek Professional Gynecological Services for specific symptoms:
- Educate women on the importance of paying attention to their bodies and recognizing symptoms that may indicate a gynecological issue. These symptoms could include abnormal bleeding, pelvic pain, unusual discharge, or changes in menstrual patterns.
- Stress the significance of not ignoring symptoms and seeking prompt medical attention to address potential problems before they escalate.
Holistic Approaches to Gynecological Health:
Discuss lifestyle factors that can positively impact gynecological health, including diet and exercise:
- A healthy lifestyle significantly contributes to gynecological well-being. Explore the role of a balanced diet in supporting hormonal balance and overall health.
- Discuss the benefits of regular exercise in maintaining a healthy weight, reducing stress, and improving circulation, all of which positively influence gynecological health.
Explore complementary therapies that may support overall well-being:
- Acknowledge that holistic well-being goes beyond traditional medical approaches. Explore complementary therapies such as acupuncture, yoga, and meditation, which can contribute to stress reduction, hormone balance, and improved mental health.
- Encourage women to find a combination of approaches that works best for them, in consultation with their healthcare provider.
Cultural and Societal Perspectives:
Address cultural taboos surrounding Professional Gynecological Services:
- Recognize that cultural taboos may prevent open discussions about gynecological health. Emphasize the importance of breaking these taboos to promote awareness, understanding, and proactive health management.
- Provide examples of how different cultures view and discuss gynecological health and encourage respectful conversations that challenge stereotypes.
Encourage open conversations and the breaking of stigmas:
- Foster an environment where women feel comfortable discussing gynecological health openly. Encourage family, friends, and community members to support one another in seeking information and healthcare.
- Emphasize that open conversations can lead to increased awareness, reduced stigma, and improved overall well-being.
Resources for Women’s Health:
- Provide information on reliable sources for women to learn more about their gynecological health:
- Direct women to reputable sources of information on the internet, such as medical websites, government health portals, and reputable health organizations. Encourage them to stay informed about the latest developments in women’s health.
- Emphasize the importance of critically evaluating information sources to ensure accuracy and reliability.
Professional Gynecological Services Include contact details for local healthcare providers and clinics:
- Offer practical information by providing contact details for local gynecologists, women’s health clinics, and community health centers. This makes it easier for women to schedule routine check-ups and seek medical advice when needed.
- Highlight the accessibility of healthcare services and the importance of establishing a relationship with a trusted healthcare provider for ongoing gynecological care.
FAQ ( Frequently Asked question)
It refers to the overall Professional Gynecological Services for the female reproductive system, including the uterus, ovaries, fallopian tubes, cervix, and vagina. It encompasses various aspects such as menstrual health, reproductive health, and the prevention and detection of diseases and conditions affecting the female reproductive organs.
Regular Professional Gynecological Services and vaccinations (such as the HPV vaccine) are key components of preventive care, helping to mitigate the risk of certain gynecological cancers and infections.
- Common menstrual disorders like irregular periods, heavy bleeding (menorrhagia), and painful periods (dysmenorrhea).
- Impact of these disorders on daily life and emphasize the importance of seeking medical advice for persistent issues.
Hormonal changes, such as those occurring during the menstrual cycle, pregnancy, and menopause, can influence mood and mental well-being.